In maxillofacial surgery, the oculocardic reflex can be occur when we explore orbit or any operation that have to associated with orbit.
-----------------------
The oculocardiac reflex, also known as Aschner phenomenon, Aschner reflex, or Aschner-Dagnini reflex, is a decrease in pulse rate associated with traction applied to extraocular muscles and/or compression of the eyeball. The reflex is mediated by nerve connections between the trigeminal cranial nerve and the vagus nerve of the parasympathetic nervous system. The afferent tracts derive mainly from the ophthalmic division of the trigeminal nerve, although tracts from the maxillary and mandibular division have also been documented[1]. These afferents synapse with the visceral motor nucleus of the vagus nerve, located in the reticular formation of the brain stem. The efferent portion is carried by the vagus nerve from the cardiovascular center of the medulla to the heart, of which increased stimulation leads to decreased output of the sinoatrial node[2]. This reflex is especially sensitive in neonates and children, and must be monitored, usually by an anaesthesiologist, during paediatric ophthalmological surgery, particularly during strabismus correction surgery[3]. However, this reflex may also occur with adults. Bradycardia, junctional rhythm, asystole, and very rarely death [4], can be induced through this reflex.
Treatment/prophylaxis
Removal of the inciting stimulus is immediately indicated, and is essential for successful termination of this reflex. The surgeon, or practitioner, working on the eye should be asked to cease their activity and release the applied pressure or traction on the eyeball. This often results in the restoration of normal sinus rhythm of the heart. If not, the use of an anti-muscarinic acetylcholine (ACh) antagonist, such as atropine or glycopyrolate, will likely successfully treat the patient and permit continuation of the surgical procedure. In extreme cases, such as the development of asystole, aggressive cardiopulmonary resuscitation may be required.
21 February 2009
oculocardiac reflex
20 February 2009
19 February 2009
fracture mandible and airway obstruction
Fracture mandible that will increase the risk of airway obstruction mostly appears in 2 form.
- Fracture bilateral symphysis of mandible
- Fracture bilateral condyle of mandible
First, the symphysis acted like free segment (coz fracture bilat.), suprahyoid muscle (ex. anterior belly of digastric) will pull this segment back, The oral cavity appeared smalller, tongue have no space to occupy. This sequence make patient difficult to breath.
Latter, the fracture of bilateral condyle of mandible, in this type when patient lie down the mandible will retrude. In the same sequence, tongue have no space to occupy and patient is hard to breath.
Thus the patients in these two type (maybe) can't lie in supine position, the best position is lie on one side or semi supine position to make sure the fracture fragment will not retrude posterior.
18 February 2009
ANATOMIC CONSIDERATIONS IN NASAL BONE FRACTURE PART II: Blood supply
The rich blood supply to the nasal region predisposes individuals to epistaxis in nasal trauma. Epistaxis can be categorized as anterior or posterior, depending on the source of bleeding. The most common location is anterior epistaxis, originating from Kiesselbach’s plexus in the anteroinferior septum, which receives its blood supply from both internal and external carotid arteries. Posterior epistaxis typically arises from branches of both the sphenopalatine and anterior ethmoidal arteries. It is less common than anterior bleeding but a more frequent cause of severe hemorrhage. Nasal hemorrhage can usually be controlled by direct manual pressure in anterior bleeds. Hemorrhage from posterior sources usually resolves spontaneously, particularly if the patient’s blood pressure is controlled. However, in persistent cases, posterior packing or Foley balloon catheterization of the nasal passage may be necessary. In the most severe cases, usually secondary to maxillary arterial sources, interventional embolization may be required. Both the ophthalmic and maxillary divisions of the trigeminal nerve supply sensation to the nose. The infratrochlear nerve provides sensation to the skin of the upper nasal dorsum and sidewalls, and the anterior ethmoidal supplies the lower dorsum and tip.
17 February 2009
ANATOMIC CONSIDERATIONS IN NASAL BONE FRACTURE PART I: Bony part
The skeletal component of the nose includes the frontal process of the maxilla, the nasal process of the frontal bone, the ethmoid, the vomer, and the nasal bones. Fractures of the nasal bones occur more commonly distally, where they are broader and thinner. Significant force is required to fracture the more proximal nasal bones, in which case injury extension into the frontal process of the maxilla and frontal bone may be present.
The cartilaginous structures include the two lower lateral cartilages, two upper lateral cartilages, and the central septal cartilage. Paired upper lateral cartilages have solid attachments to the caudal aspect of the nasal bones and help maintain the midline location of the quadrangular cartilage. The lower lateral cartilages provide little midline
structural support but are responsible for much of the aesthetics and contour of the nasal tip. The fact that cartilage surrounds the bony matrix both dorsally and laterally to provide a soft and malleable framework allows some dissipation of force without incurring a permanent deformity. In general, significant force is required for a cartilaginous
injury.
12 February 2009
temporal branch of facial nerve injury (danger zone)
The temporal branch of the facial nerve is at greatest risk for injury where it crosses the zygomatic arch. Injury to the temporal branch of the facial nerve leads to an inability to elevate the eyebrows and brow ptosis and paralysis. Asymmetric appearance of the forehead can also occur because there will be a loss of the lines and wrinkles on the affected side. One easy method to delineate the danger area of the temporal nerve is to draw a line from the earlobe to the lateral edge of the eyebrow, and the tragus to just above and behind the highest forehead crease(or 2 cm above supraorbital rim). In the area between these lines , the nerve is superficial, and it is critical to undermine just below the dermis in the superficial fat above the fascia.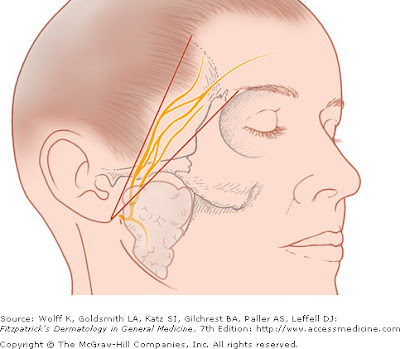
Relate posted
07 February 2009
x-ray and fracture line part 2
This post will show the radiographic sign that I tell you in x-ray and fracture line posted
The figure below shows the oblique fracture that the fracture fragment was oblique and overlapped in bucco-lingual direction, thus, show the more radiopaque line (red arrow)
The next picture shows topographic view of the same case, the fracture fragment was overlapped from 44-47 area.
This last picture shows the fracture of right zygomatic arch. The arch was overlapped (in superior-inferior and medial-distal direction), thus it show more radiopaque and more widening than normal side.
Relate posted