In maxillofacial surgery, the oculocardic reflex can be occur when we explore orbit or any operation that have to associated with orbit.
-----------------------
The oculocardiac reflex, also known as Aschner phenomenon, Aschner reflex, or Aschner-Dagnini reflex, is a decrease in pulse rate associated with traction applied to extraocular muscles and/or compression of the eyeball. The reflex is mediated by nerve connections between the trigeminal cranial nerve and the vagus nerve of the parasympathetic nervous system. The afferent tracts derive mainly from the ophthalmic division of the trigeminal nerve, although tracts from the maxillary and mandibular division have also been documented[1]. These afferents synapse with the visceral motor nucleus of the vagus nerve, located in the reticular formation of the brain stem. The efferent portion is carried by the vagus nerve from the cardiovascular center of the medulla to the heart, of which increased stimulation leads to decreased output of the sinoatrial node[2]. This reflex is especially sensitive in neonates and children, and must be monitored, usually by an anaesthesiologist, during paediatric ophthalmological surgery, particularly during strabismus correction surgery[3]. However, this reflex may also occur with adults. Bradycardia, junctional rhythm, asystole, and very rarely death [4], can be induced through this reflex.
Treatment/prophylaxis
Removal of the inciting stimulus is immediately indicated, and is essential for successful termination of this reflex. The surgeon, or practitioner, working on the eye should be asked to cease their activity and release the applied pressure or traction on the eyeball. This often results in the restoration of normal sinus rhythm of the heart. If not, the use of an anti-muscarinic acetylcholine (ACh) antagonist, such as atropine or glycopyrolate, will likely successfully treat the patient and permit continuation of the surgical procedure. In extreme cases, such as the development of asystole, aggressive cardiopulmonary resuscitation may be required.
21 February 2009
oculocardiac reflex
20 February 2009
19 February 2009
fracture mandible and airway obstruction
Fracture mandible that will increase the risk of airway obstruction mostly appears in 2 form.
- Fracture bilateral symphysis of mandible
- Fracture bilateral condyle of mandible
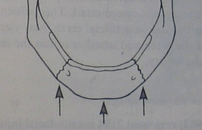
First, the symphysis acted like free segment (coz fracture bilat.), suprahyoid muscle (ex. anterior belly of digastric) will pull this segment back, The oral cavity appeared smalller, tongue have no space to occupy. This sequence make patient difficult to breath.
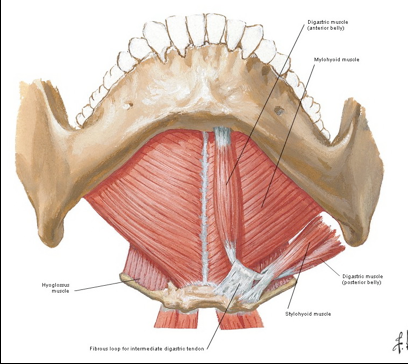
Latter, the fracture of bilateral condyle of mandible, in this type when patient lie down the mandible will retrude. In the same sequence, tongue have no space to occupy and patient is hard to breath.
Thus the patients in these two type (maybe) can't lie in supine position, the best position is lie on one side or semi supine position to make sure the fracture fragment will not retrude posterior.
18 February 2009
ANATOMIC CONSIDERATIONS IN NASAL BONE FRACTURE PART II: Blood supply
The rich blood supply to the nasal region predisposes individuals to epistaxis in nasal trauma. Epistaxis can be categorized as anterior or posterior, depending on the source of bleeding. The most common location is anterior epistaxis, originating from Kiesselbach’s plexus in the anteroinferior septum, which receives its blood supply from both internal and external carotid arteries. Posterior epistaxis typically arises from branches of both the sphenopalatine and anterior ethmoidal arteries. It is less common than anterior bleeding but a more frequent cause of severe hemorrhage. Nasal hemorrhage can usually be controlled by direct manual pressure in anterior bleeds. Hemorrhage from posterior sources usually resolves spontaneously, particularly if the patient’s blood pressure is controlled. However, in persistent cases, posterior packing or Foley balloon catheterization of the nasal passage may be necessary. In the most severe cases, usually secondary to maxillary arterial sources, interventional embolization may be required. Both the ophthalmic and maxillary divisions of the trigeminal nerve supply sensation to the nose. The infratrochlear nerve provides sensation to the skin of the upper nasal dorsum and sidewalls, and the anterior ethmoidal supplies the lower dorsum and tip.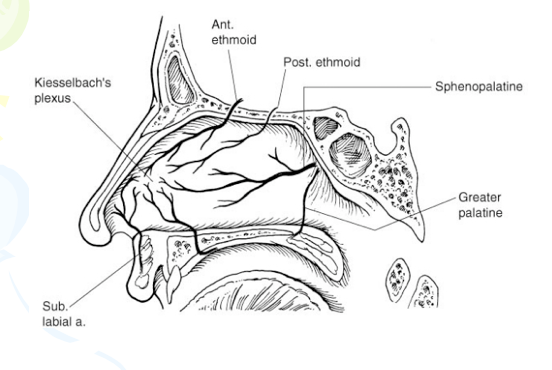
17 February 2009
ANATOMIC CONSIDERATIONS IN NASAL BONE FRACTURE PART I: Bony part
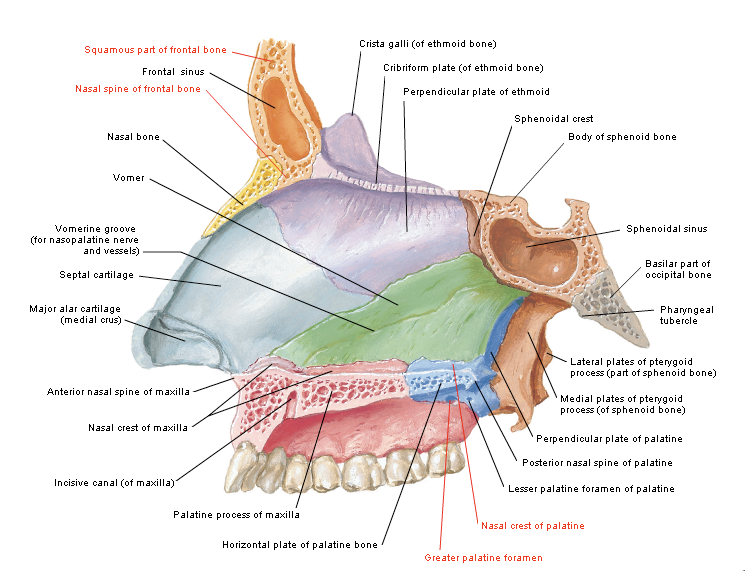
The skeletal component of the nose includes the frontal process of the maxilla, the nasal process of the frontal bone, the ethmoid, the vomer, and the nasal bones. Fractures of the nasal bones occur more commonly distally, where they are broader and thinner. Significant force is required to fracture the more proximal nasal bones, in which case injury extension into the frontal process of the maxilla and frontal bone may be present.
The cartilaginous structures include the two lower lateral cartilages, two upper lateral cartilages, and the central septal cartilage. Paired upper lateral cartilages have solid attachments to the caudal aspect of the nasal bones and help maintain the midline location of the quadrangular cartilage. The lower lateral cartilages provide little midline
structural support but are responsible for much of the aesthetics and contour of the nasal tip. The fact that cartilage surrounds the bony matrix both dorsally and laterally to provide a soft and malleable framework allows some dissipation of force without incurring a permanent deformity. In general, significant force is required for a cartilaginous
injury.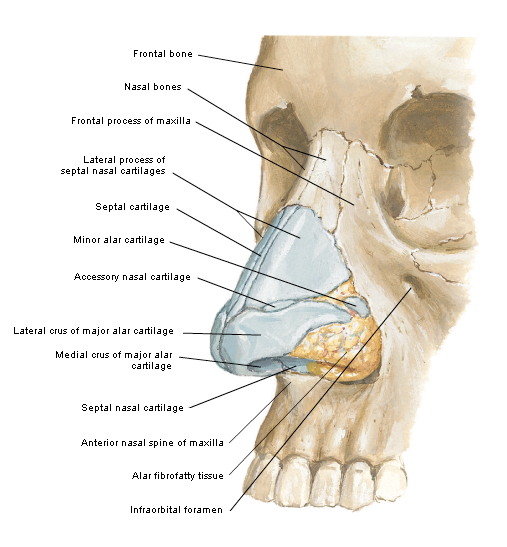
12 February 2009
temporal branch of facial nerve injury (danger zone)
The temporal branch of the facial nerve is at greatest risk for injury where it crosses the zygomatic arch. Injury to the temporal branch of the facial nerve leads to an inability to elevate the eyebrows and brow ptosis and paralysis. Asymmetric appearance of the forehead can also occur because there will be a loss of the lines and wrinkles on the affected side. One easy method to delineate the danger area of the temporal nerve is to draw a line from the earlobe to the lateral edge of the eyebrow, and the tragus to just above and behind the highest forehead crease(or 2 cm above supraorbital rim). In the area between these lines , the nerve is superficial, and it is critical to undermine just below the dermis in the superficial fat above the fascia.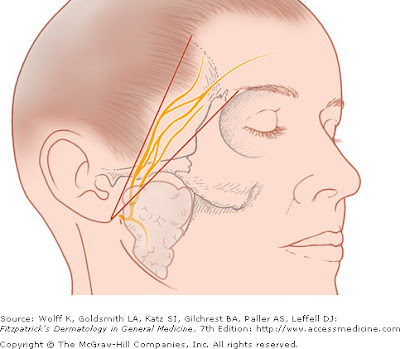
Relate posted
07 February 2009
x-ray and fracture line part 2
This post will show the radiographic sign that I tell you in x-ray and fracture line posted
The figure below shows the oblique fracture that the fracture fragment was oblique and overlapped in bucco-lingual direction, thus, show the more radiopaque line (red arrow)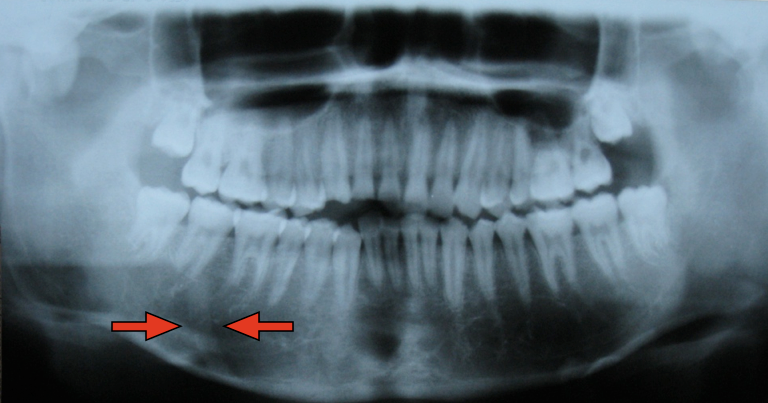
The next picture shows topographic view of the same case, the fracture fragment was overlapped from 44-47 area.
This last picture shows the fracture of right zygomatic arch. The arch was overlapped (in superior-inferior and medial-distal direction), thus it show more radiopaque and more widening than normal side.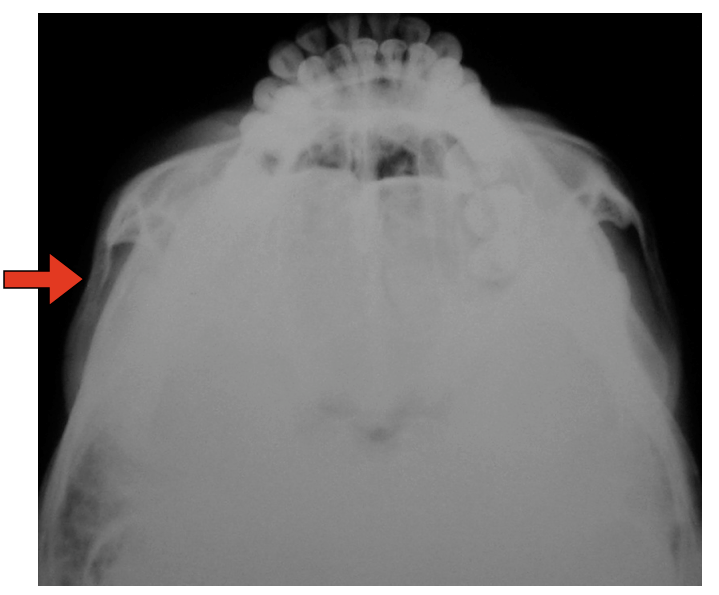
Relate posted
05 February 2009
x-ray and fracture line
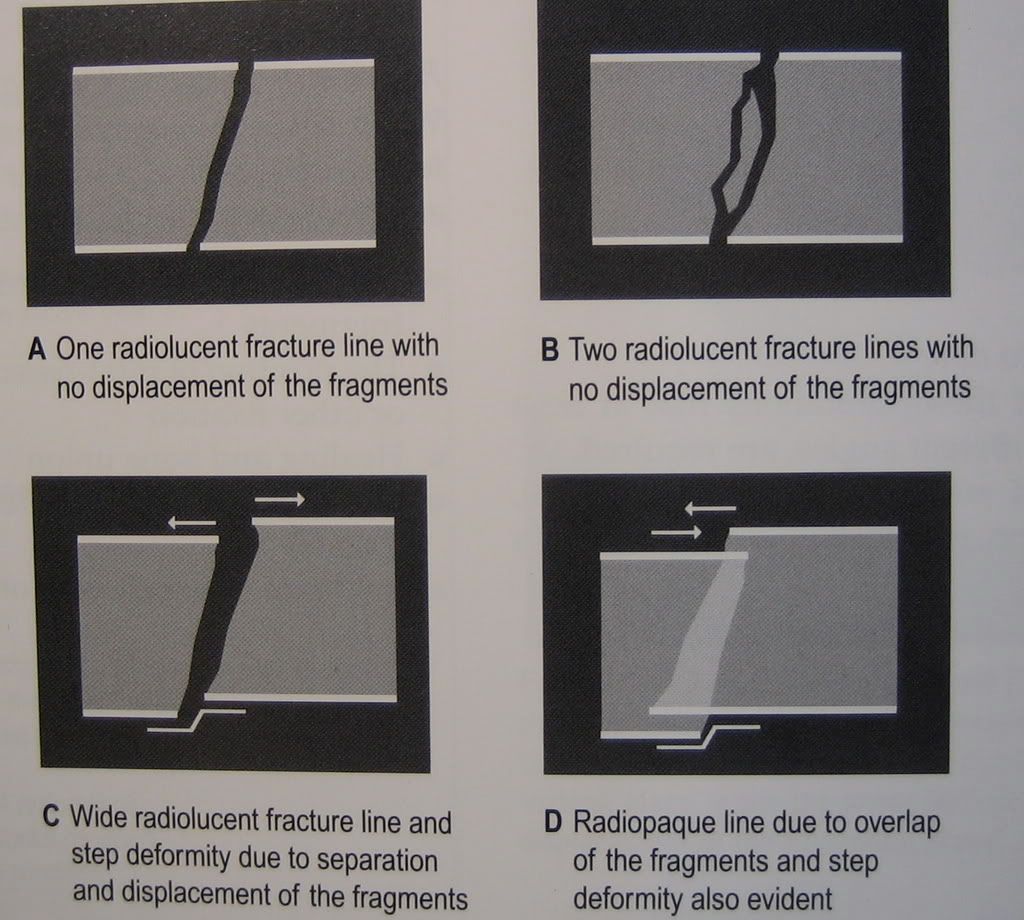
The typical x-ray appearances of fracture included
- Radiolucent line
- Radiopaque line if the fragments overlie one another
- Discontinuity or deformity in the out line of the bone
Why can we see more radiopaque line in fracture look at this figure below?
For example, the oblique fracture of mandible ,we will didn't notice in x-ray because it sometimes presented only slightly not notably more radiopaque line. (The fracture fragment was overlapped)
Another example, in submentovertex view, in fracture zygomatic arch that the arch was collapsed and overlapped, show only slightly increase of radiopaque and widening of arch than contralateral arch.
Next time if I 'm not forget I will show the example of these film x-ray, however the most important in diagnosis the fracture of head and neck bone was not x-ray, but clinical.
Relate posted
04 February 2009
What is osteoradionecrosis (ORN) ?
Osteoradionecrosis easy definition is
1. Patient who previously recieve radiotherapy > 5000 rad
2. Bone exposed with non healing > 3 month
Stage of Osteoradionecrosis -- ORN
Osteoradionecrosis (ORN) can divided into 3 stage
Stage 1 is superficial osteoradionecrosis that can resolve with irrigation and hyperbaric oxygen (HBO)
In stage 1 osteoradionecrosis no bone surgical removal is required.
Stage 2 is stage 1 that progressive and can't healing with treatment method in stage 1
Stage 3 is ORN that have orocutaneous fistula, Pathologic fracture or resorption of inferior border of mandible.
We have to known each stage of ORN for effective treatment protocol that I show below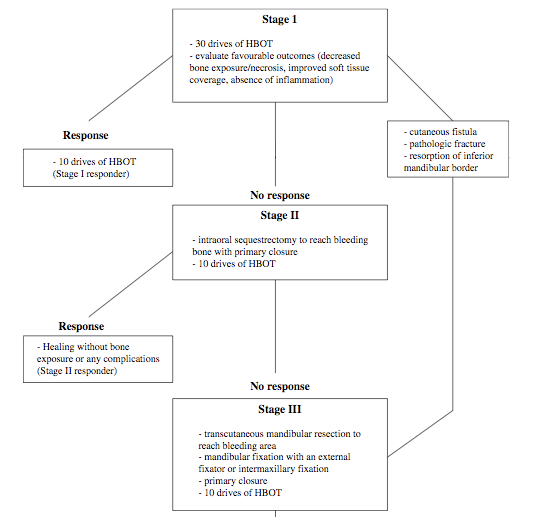
For full description of 3 stage of osteoradionecrosis read below.
-----------------------------------------------
ORN Staging System
Stage I
All patients who meet the definition of osteoradionecrosis except those with cutaneous
fistulae, pathologic fracture, or radiographic evidence of bone resorption. (These three
subsets of patients are classified as Stage III.) Stage I patients receive 30 HBOT
treatments. Wounds are maintained with irrigation only or with saline rinses. No bone is
surgically removed. If, after 30 treatments, the wound shows improvement, as evidenced
by decrease in amount of exposed bone; less resporption or spontaneous sequestration of
exposed bone; or decreased softening of exposed bone; the patient completes another 10
treatments. The total 40 HBOT treatments are meant to achieve full mucosal cover. If
there is no clinical improvement after 30 HBOT treatments or complete resolution, such
as extended or continued exposure of bone, absence of mucosal proliferation, or presence
of inflammation, the patient is advanced further to Stage II. (See Technical Treatment
Protocol for suggestions on pressure levels and duration of individual treatments.)
Stage II
Surgeons attempt a local surgical debridement to identify those patients with only
superficial or cortical bone involvement, and who can be resolved without jaw resection.
A transoral alveolar sequestrectomy is performed with fine saline-cooled, air-driven
saws. Minimal periosteal manipulation is done for labial access to the mandible. The
lingual periosteum is allowed to remain completely attached until the specimen is
delivered, and then only that which is attached to the specimen is reflected from bone.
The resultant mucoperiosteal flaps are closed in three layers over a base of bleeding bone.
If healing progresses without complication, HBOT is continued with 10 additional
sessions. If the wound dehisces, leaving exposed non-healing bone, the patient isadvanced to Stage III. In those patients who initially present with orocutaneous fistulae,
with pathologic fracture, or with radiographic osteolysis to the inferior border, the initial
30 HBOT treatments are given, and the patient enters Stage III directly.
Stage III
After 30 HBOT treatments, the patient undergoes a transoral partial jaw resection, the
margins of which are determined at the time of surgery by the presence of bleeding bone. The segments of the mandible are stabilized either with extraskeletal pin fixation or with maxillo mandibular fixation. If there was an orocutaneous fistula, or large soft tissue loss, primary closure or soft-tissue reconstruction is accomplished during this surgery. HBOT is continued for another 10 treatments, and the patient is advanced to Stage III-R.
Stage III-R
These patients present the most difficult cases. Early reconstruction and rehabilitation
produces the best results. Ten weeks after resection, the soft tissues are healing, and the potential graft bed is free from contamination and infection. Bony reconstruction is
undertaken from a strictly transutaneous approach without oral flora contamination.
Ten post-reconstructive HBOT treatments are given, and the jaw fixation is maintained
for eight weeks. If no further surgery is required, the patient begins appointments with a
maxillofacial prosthodontist for full prosthetic rehabilitation one month after release of
his fixation. If additional surgery is required, such as a tongue release, vestibuloplasty, or excision of redundant tissue, surgeons schedule procedures one month after fixation is released. After surgery, the patient is referred to a maxillofacial prosthodontist.
02 February 2009
Tear lacrimal canaliculi injury
Lacrimal canaliculi injury can be occur in head and neck injury and have to specially suspected in patient that have laceration wound at eyelid involve lid margin.
See the picture of lacrimal duct system, the vertical part of canaliculi about 2 mm and horizontal part about 8 mm, thus the laceration wound in range about 5-10 mm from medial palpebral fissure have highly incident of lacrimal canaliculi injury. (the injury that medial to the punctum of eye.)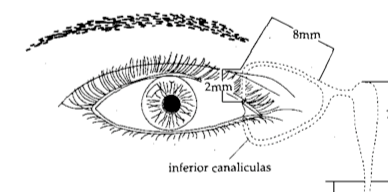
Lacrimal canaliculi have both at upper and lower lid margin, the openning is through the upper and lower punctum. The percent of tear drainage are 75% from lower canaliculi and remaining for upper canaliculi. The main is at lower lacrimal canaliculi. If it have injury to this canaliculi and we didn't repair it the tear will can't drain and epiphora will occur.

Next post I will show method to repair canaliculi.
See ya.
01 February 2009
CA node metastasis or not
How to know this is CA metastasis node or not?
- Found primary CA
- Fix node (You have to try move node in every direction to confirm it fix or not)
- Node diameter > 1 cm
- Chain node (In viral infection also have chain node, but viral infection will have prodormal sign)
- Node was no tender (In general, infection node will have tenderness, anyway, chronic infection will also absence of tenderness.)
It just the consideration point to determine that is it CA metastasis node or not.