osteoradionecrosis เราสามารถแบ่งออกเป็นทั้งหมด 3 stage โดย stage III ตามตัวหนังสือที่เขียนไว้ก็คือ ลักษณะของ ORN ร่วมกับมี fistula opening หรือมี pathologic fracture ของตัวกระดูกร่วมด้วย ซึ่งถ้าเราแบ่ง stage ของ ORN ตามลักษณะของมันนั้น เราจะยังเข้าไม่ถึงหัวใจของการแบ่ง ORN
อธิบายอีกทางก็คือ สมมุติเราพบ ORN ที่มี fistula openning แต่เราส่งไปทำ HBO แล้วอาการผู้ป่วย response ดีขึ้นจนหายดีโดยเราไม่ต้องทำ intervention ใดๆเลย เรายังจะให้เป็น ORN stage III หรือไม่
ดังนั้น จริงๆแล้วการแบ่ง stage ORN อย่างง่ายๆเลยก็คือ ถ้า ORN ที่ response ต่อ HBO 3o drive แล้วสามารถรักษาหายได้โดยไม่ต้องทำ local debridement ใด เราถือว่าเป็น stage I แต่ถ้าได้ HBO 30 drive อาการไม่ดีขึ้น ต้องทำ local debridement แล้วรักษาหายได้ เราถือว่าเป็น ORN stage II และสุดท้ายถ้ารักษาด้วยการ local debridement ไม่หาย ต้องใช้การรักษาที่ aggressive มากขึ้นไปอีก เราก็จะถือว่ามันเป็น ORN stage III
11 March 2009
staging of osteoradio necrosis (ORN)
04 February 2009
What is osteoradionecrosis (ORN) ?
Osteoradionecrosis easy definition is
1. Patient who previously recieve radiotherapy > 5000 rad
2. Bone exposed with non healing > 3 month
Stage of Osteoradionecrosis -- ORN
Osteoradionecrosis (ORN) can divided into 3 stage
Stage 1 is superficial osteoradionecrosis that can resolve with irrigation and hyperbaric oxygen (HBO)
In stage 1 osteoradionecrosis no bone surgical removal is required.
Stage 2 is stage 1 that progressive and can't healing with treatment method in stage 1
Stage 3 is ORN that have orocutaneous fistula, Pathologic fracture or resorption of inferior border of mandible.
We have to known each stage of ORN for effective treatment protocol that I show below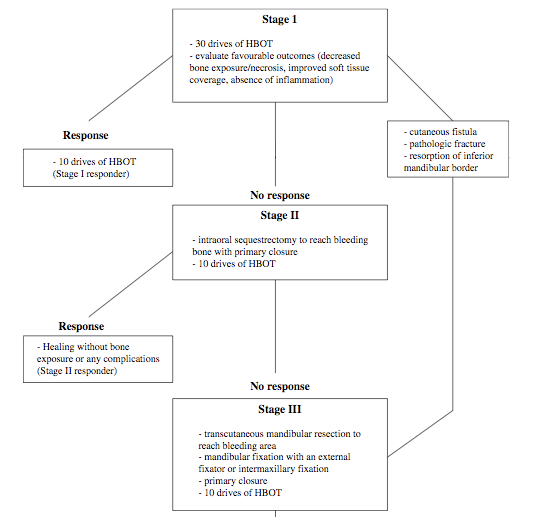
For full description of 3 stage of osteoradionecrosis read below.
-----------------------------------------------
ORN Staging System
Stage I
All patients who meet the definition of osteoradionecrosis except those with cutaneous
fistulae, pathologic fracture, or radiographic evidence of bone resorption. (These three
subsets of patients are classified as Stage III.) Stage I patients receive 30 HBOT
treatments. Wounds are maintained with irrigation only or with saline rinses. No bone is
surgically removed. If, after 30 treatments, the wound shows improvement, as evidenced
by decrease in amount of exposed bone; less resporption or spontaneous sequestration of
exposed bone; or decreased softening of exposed bone; the patient completes another 10
treatments. The total 40 HBOT treatments are meant to achieve full mucosal cover. If
there is no clinical improvement after 30 HBOT treatments or complete resolution, such
as extended or continued exposure of bone, absence of mucosal proliferation, or presence
of inflammation, the patient is advanced further to Stage II. (See Technical Treatment
Protocol for suggestions on pressure levels and duration of individual treatments.)
Stage II
Surgeons attempt a local surgical debridement to identify those patients with only
superficial or cortical bone involvement, and who can be resolved without jaw resection.
A transoral alveolar sequestrectomy is performed with fine saline-cooled, air-driven
saws. Minimal periosteal manipulation is done for labial access to the mandible. The
lingual periosteum is allowed to remain completely attached until the specimen is
delivered, and then only that which is attached to the specimen is reflected from bone.
The resultant mucoperiosteal flaps are closed in three layers over a base of bleeding bone.
If healing progresses without complication, HBOT is continued with 10 additional
sessions. If the wound dehisces, leaving exposed non-healing bone, the patient isadvanced to Stage III. In those patients who initially present with orocutaneous fistulae,
with pathologic fracture, or with radiographic osteolysis to the inferior border, the initial
30 HBOT treatments are given, and the patient enters Stage III directly.
Stage III
After 30 HBOT treatments, the patient undergoes a transoral partial jaw resection, the
margins of which are determined at the time of surgery by the presence of bleeding bone. The segments of the mandible are stabilized either with extraskeletal pin fixation or with maxillo mandibular fixation. If there was an orocutaneous fistula, or large soft tissue loss, primary closure or soft-tissue reconstruction is accomplished during this surgery. HBOT is continued for another 10 treatments, and the patient is advanced to Stage III-R.
Stage III-R
These patients present the most difficult cases. Early reconstruction and rehabilitation
produces the best results. Ten weeks after resection, the soft tissues are healing, and the potential graft bed is free from contamination and infection. Bony reconstruction is
undertaken from a strictly transutaneous approach without oral flora contamination.
Ten post-reconstructive HBOT treatments are given, and the jaw fixation is maintained
for eight weeks. If no further surgery is required, the patient begins appointments with a
maxillofacial prosthodontist for full prosthetic rehabilitation one month after release of
his fixation. If additional surgery is required, such as a tongue release, vestibuloplasty, or excision of redundant tissue, surgeons schedule procedures one month after fixation is released. After surgery, the patient is referred to a maxillofacial prosthodontist.